Exosomes Deliver Potent Chemotherapeutic Agent to Cancer Cells
Researchers from the University of North Carolina (UNC) at Chapel Hill have increased the effectiveness of a chemotherapeutic agent 50 fold. The drug, paclitaxel (PTX), was introduced in exosomes that were delivered to cells and mice affected by multidrug resistant (MDR) cancer. The exosomes avoided the drug’s degradation by the immune system. The study was published in the journal Nanomedicine: Nanotechnology, Biology and Medicine.
Most chemotherapeutic agents are cytotoxic compounds that attack actively-dividing cells -a characteristic of cancer cells. This results in healthy, rapidly-dividing cells being destroyed along with cancer cells. Researchers have been trying to find a way to deliver chemotherapeutic agents with higher precision, and over the last decade several artificial nanoparticles have been used to encapsulate anti-cancer drugs and deliver them to cancer cells. Packaging the drug also has the purpose of hiding it from the body’s immune system, avoiding its degradation and the subsequent need of large doses -which increase side effects.
Exosomes from white blood cells loaded with anti-cancer drugs
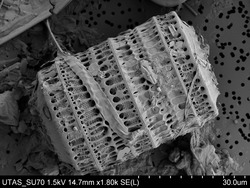
Exosomes are lipidic vesicles used by cells to transport molecules to the extracellular space and to other cells, with important functions in intercellular communication. The researchers from UNC decided to extract exosomes from white blood cells and introduced the drug PTX inside them by sonication. After the vesicle membrane was reconstituted, the PTX-filled exosomes (exoPTX) were delivered to MDR cancer cells cultured in vitro. ExoPTX vesicles successfully entered the cells, increasing citotoxicity more than 50 times compared to non-exosome-mediated PTX delivery. ExoPTX vesicles were then loaded with dye and introduced in mice affected by drug-resistant lung cancer. The vesicles marked the cancer cells and eliminated them with great efficiency, working both as a diagnostic tool and a therapeutic agent.
This study opens the door to the use of more potent chemotherapeutic agents at much lower doses, increasing their effectiveness and diminishing unwanted side effects.
Source: UNC