Pancreatic Cells Originated from Human Skin Revert Diabetes in Mice

Researchers from the Gladstone Institutes and the University of California, San Francisco (UCSF) have created for the first time functional pancreatic cells from human skin cells. Diabetic mice transplanted with the insuline-producing cells could control their glucose levels. The innovative cell reprogramming protocol will allow to scale up cell production and use them in disease modelling, drug screening and, potentially, cell therapy. The study was published in Nature Communications.
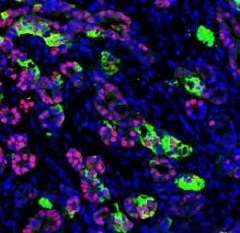
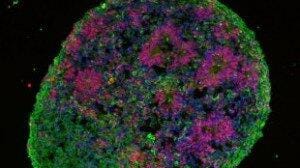
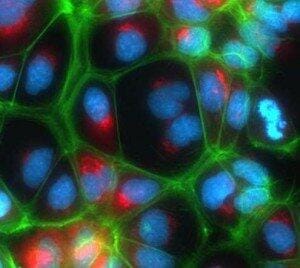
The main goal of regenerative medicine is to obtain functional cells and organoids to test drugs and model diseases. The production of pancreatic cells would be very advantageous for the study of diabetes. Several methods have been used in the past to reprogram human embryonic stem cells and induced pluripotent stem cells into beta cells, which make up to 80% of the pancreatic islets. However, a protocol to produce high numbers of pancreatic beta cells was still lacking. Taking a different approach, Sheng Ding and his team decided to revert adult skin cells into endoderm cells, a cell lineage known to originate all cells from the gastrointestinal and respiratory tracks, among other specific cell types. This has the advantage of not having to take the adult cells back to a pluripotent state, saving time. More importantly, cells proliferate extensively at the endoderm stage, before differentiating into the desired type. By overexpressing pluripotent transcription factors together with lineage specific signals, the team was able to reprogram mouse fibroblasts into several cell types, pancreatic cells among them. Unfortunately, the method couldn’t generate functional human beta cells that reversed diabetes in mice.
Trillion-fold increase at endoderm stage
In their last study, Sheng Ding and his coworkers reprogrammed human adult and neonatal fibroblasts into endoderm cells using reprogramming and specific growth factors in a non-integrative way. They also identified the molecules that allow for greater proliferation of reprogrammed cells at different developmental stages. Following this new protocol, they produced functional beta cells in vitro that also protected mice from diabetes when transplanted.
The new method by Sheng Ding’s lab for generating human pancreatic beta cells paves the way for the in vitro production of relevant quantities of lineage-specific cells that can be later programmed to become any desired cell type. Patient-specific cells can be generated to perform in vitro disease studies and drug screenings.
Source: Gladstone