Micro-hearts Obtained In Vitro by Physical Confinement
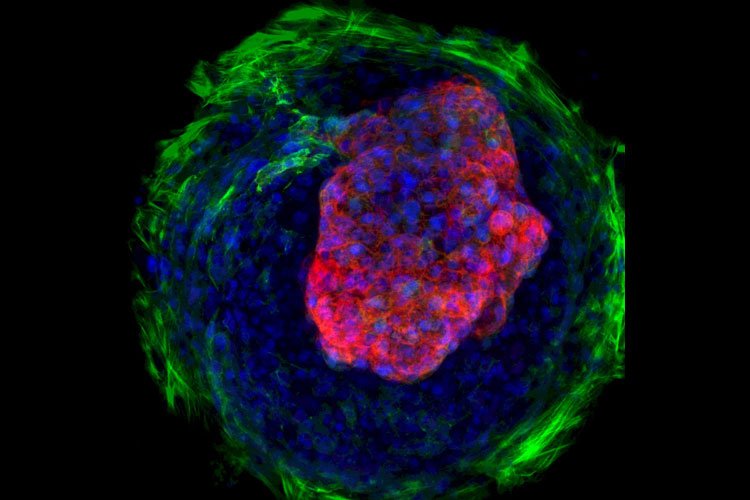
Researchers from the University of California in Berkeley and San Francisco have obtained cardiac microchambers in vitro by confining their space. It is the first time an organ is obtained without a preexisting extracellular scaffold. The team restricted the cells space using patterned substrates, and this resulted in cell lineage differentiation and eventually in the formation of cardiac microchambers. These micro-hearts will be used to study cardiac development and drug toxicity. The study was published in Nature Communications.
The biophysical properties of tissue patterning are long known to be important for tissue development. The form of the embryo and the adult phenotype depend on signal transduction, that is, on molecules interacting with cell receptors, creating a cascade of events and eventually a response. But biomechanical processes, governed by physics, are also important. Cells sense forces and biophysical properties of their environment. That information is transmitted through signal pathways and affects tissue morphogenesis.
Complex biophysical interactions are difficult to model. An emerging field plays with the extracellular substrate´s physical properties to control cell differentiation. Properties such as substrate stiffness or surface topography are modified and the consequences are studied.
Confinement conditions cell development
The authors of this study had previously been able to generate cardiac tissue in vitro. From human induced pluripotent stem cells (hiPSCs), they obtained embryoid bodies, which are three-dimensional aggregates of pluripotent stem cells. These bodies spontaneously vascularized and developed into cardiac tissue. However, in the artificial environment, the cells lacked the natural mechanical input. This made in vitro experiments hardly reproducible. To solve this problem, the current study introduced biophysical cues: Healy´s team patterned the substrate during the differentation process. As a result of the confinement information, -the creation of non-accessible zones that imitate natural physical constraints-, cells differentiated into different lineages. Central cells turned into beating cardiomyocites, and the surrounding cells became fibroblasts. Eventually cardiac microchambers were formed, which serve as heart development models. The researchers showed the clinical potential of the microchambers by running a drug-screening on them. Micro-hearts will allow to perform safe tests on medications meant to be taken by pregnant women. The experience with micro-hearts will also be key for creating a real heart from self-organising cells.